Why Run a Functional Food Sensitivity Test?
What are we testing?
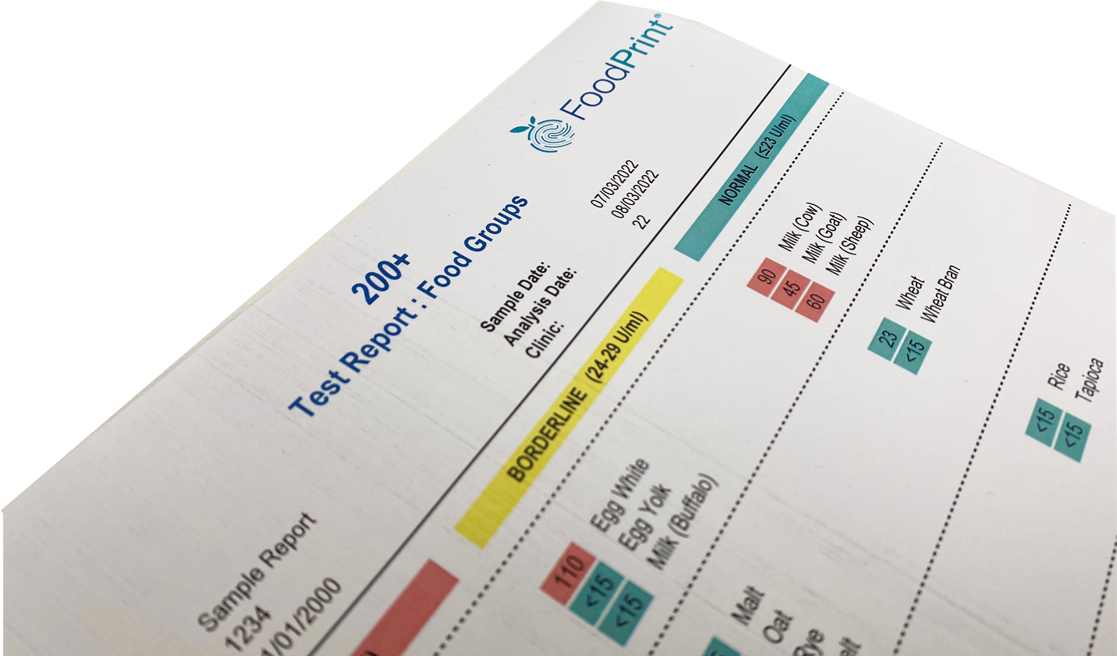
An IgG food sensitivity test (FST) assesses delayed immune responses to foods. IgG immune responses are an overlooked potential cause of inflammatory reactions which manifest in a variety of systemic symptoms and diseases.
Testing is a valuable client-specific tool to guide protocol, particularly the construction of bespoke meal plans, avoiding incorrect dietary management which may both contribute to and amplify symptoms.
This test is not an IgE allergy test, nor an intolerance test.
IgG antibodies are raised to specific proteins (antigens) in foods once digested, some of which may stimulate an immune response. The immune response for each person varies, and whilst some foods are commonly positive, results show high level of personalisation. Symptom presentation may be delayed by up to 3 to 5 days.
Overlooked potential cause of symptoms
Patients clinically presenting with allergic symptoms are usually investigated for the presence of specific IgE antibodies that may not be present among a subgroup of patients presenting with symptoms due to IgG food sensitivities. When IgE is the only route pursued, a group of patients may not only remain undiagnosed, but also continue to suffer from preventable symptoms (1).
Association with functional gut testing
Diet and lifestyle stressors are increasingly recognised as contributing factors towards the breakdown of epithelial cell wall integrity, commonly termed intestinal permeability, or leaky gut. Once this vital first line immune defence system is breached, poorly digested foods, along with pathogens including viruses, bacteria, and endotoxins, gain access to the body stimulating unwanted immune responses, inflammation, and symptoms.
Although producing IgG antibodies is a normal defence reaction to foods, abnormally high levels signify disruption or loss of tolerance (2). Alongside a functional gut test, and in an era of personalised nutrition, an IgG FST provides a diagnostic solution backed by scientific expertise to support a unique management strategy. Test now to regain balance and tolerance.
When to test
Scientific evidence supports the use of food-specific IgG elimination diets related to the following conditions:
GASTROINTESTINAL
(relating to symptoms including bloating, pain, gas, diarrhoea, constipation, inconsistent stools, irritable bowel syndrome (IBS) and inflammatory bowel diseases (IBD))
• Inflammatory Bowel Disease (IBD): Ulcerative Colitis (UC) And Crohn’s Disease (CD)
IgG-guided exclusion diets may ameliorate ulcerative colitis symptoms and improve quality of life (3). In one study, elevated food IgG antibodies were detected in 75.9% of CD patients, and 63.6% of UC patients, compared with 33.1% of healthy controls. Levels of IgG antibodies may potentially indicate disease status and be used to guide clinical diets (4).
• Irritable Bowel Syndrome (IBS) (affecting 12-20% of the population)
Most patients with IBS attribute their symptoms to adverse food reactions (5, 6) and serum IgG levels are higher in patients with IBS and a food allergy history, potentially related to an inflamed or leaky gut (7). But the increase of food-specific IgG antibodies could be a specific reaction, rather than a non-specific response to increased gut mucosal permeability (8, 9).
• IBS And Athletic Performance
A 3-month elimination diet decreased chronic inflammation of the GI tract and exerted a significant influence on the athletes’ body composition, with indirect improvement to their sports performance (10).
• IBS: Comparison with FODMAP Diets
When compared with the FODMAP diet, IgG elimination-rotation diets were found to be more effective in the treatment of patients with mixed IBS (11).
• IBS and Mast Cell Activation
There may be a plausible link between mast cell activation in the gut, stimulated by food-specific IgG antibodies, and IBS symptoms (12). Skin symptoms e.g., wheals, redness and itching, may also be noted.
• Intestinal Permeability/Leaky Gut
Elevated food-specific IgG antibodies may be present in conjunction with increased concentrations of intestinal permeability biomarkers. Common highly reactive foods like wheat, dairy, and eggs may be the drivers (13).
AUTOIMMUNE AND CHRONIC CONDITIONS
(symptoms include skin problems, joint pain, swelling, arthritic conditions, stiffness, low energy, fatigue, hair loss, ulcers)
Bespoke elimination diets, as compared to generically restricted diets, highlight significant therapeutic benefits relevant to all chronic health conditions and foods may be an important trigger for autoimmunity in vulnerable patients. Foods such as casein, cow’s milk, wheat, gliadin, and egg white repeatedly showing up as key culprits (14).
Hardman demonstrated that 75.8% of participants noted improvements in their various health conditions following an IgG guided elimination diet. However, 92% saw a return in symptoms when the offending foods were reintroduced. In another, involving a subset of patients with chronic, disabling symptoms, unresponsive to other intensive treatments, 20% obtained 100% relief (15).
NEUROLOGICAL
(headache, migraine, anxiety, depression, low mood state, low enthusiasm)
• Depression
Raised histamine levels in depressed adolescents correlated with raised IgG levels implicating the correlation between elevated histamine and hyperpermeability of the blood-brain barrier, implicated in the pathogenesis of Major Depressive Disorder (MMD) (17).
There is an increasing amount of evidence which links the pathogenesis of irritable bowel syndrome (IBS) with food IgG hyperreactivity. Some authors have suggested that food IgG hyperreactivity could be also involved in the pathophysiology of MDD (18).
• Migraine (reducing frequency and severity)
Migraine patients with raised food specific IgG antibodies had worse migraine, anxiety, and gastrointestinal symptoms along with elevated inflammatory cytokines (19). Increase serotonin levels were noted using an elimination diet and an elimination diet with probiotic use and a reduction in IBS and migraine scores XIE and diet restriction based on IgG antibodies is an effective strategy in reducing the frequency of migraine attack (20).
• Autism
Elevated IgG antibodies have been noted in children with autistic spectrum disorders contributing to impaired intestinal barrier function (21) seen in 25.6% of ASDS compared with 2.3% of healthy children.
WEIGHT/OBESITY
Raised IgG levels correlated with imbalanced cytokine levels indicating an inflammatory component to obesity and a potential avenue of preventative treatment for metabolic syndrome (22), weight loss in obese juveniles (23) and weight loss not unresponsive to low calorie diets (24).
RESPIRATORY
(symptoms include asthma, tight chest, rhinitis)
• Asthma
Elimination diets resulting in both a reduction in asthma symptoms and reduced pharmacological interventions (25).
SKIN
(symptoms include Itchy skin, eczema, psoriasis, dermatitis, hives, swelling, liver spots, acne)
• Eczema and Atopic Dermatitis
Raised IgG food antibody levels in children with eczema is as high as 89.35% (26, 27) and elimination diets may prove a valuable treatment tool. Antibodies to milk and eggs were particularly raised (28).
(References available on request)