The Connection Between Food Sensitivity and Leaky Gut

What is IgG-mediated sensitivity?
There is a widespread erroneous belief that immune system reactions to the foods we eat are exclusively associated with IgE antibody mediated mechanisms (true allergy). However, according to more recent studies, IgG-dependent hypersensitivity, characterised by a delayed immune response, also plays a significant role in the pathogenesis of food reactions, often referred to as ‘food sensitivity’. Testing for IgG food antibodies opens new diagnostic pathways for patients who are reacting to food and allows for a focused elimination diet, based on IgG antibodies to be implemented.
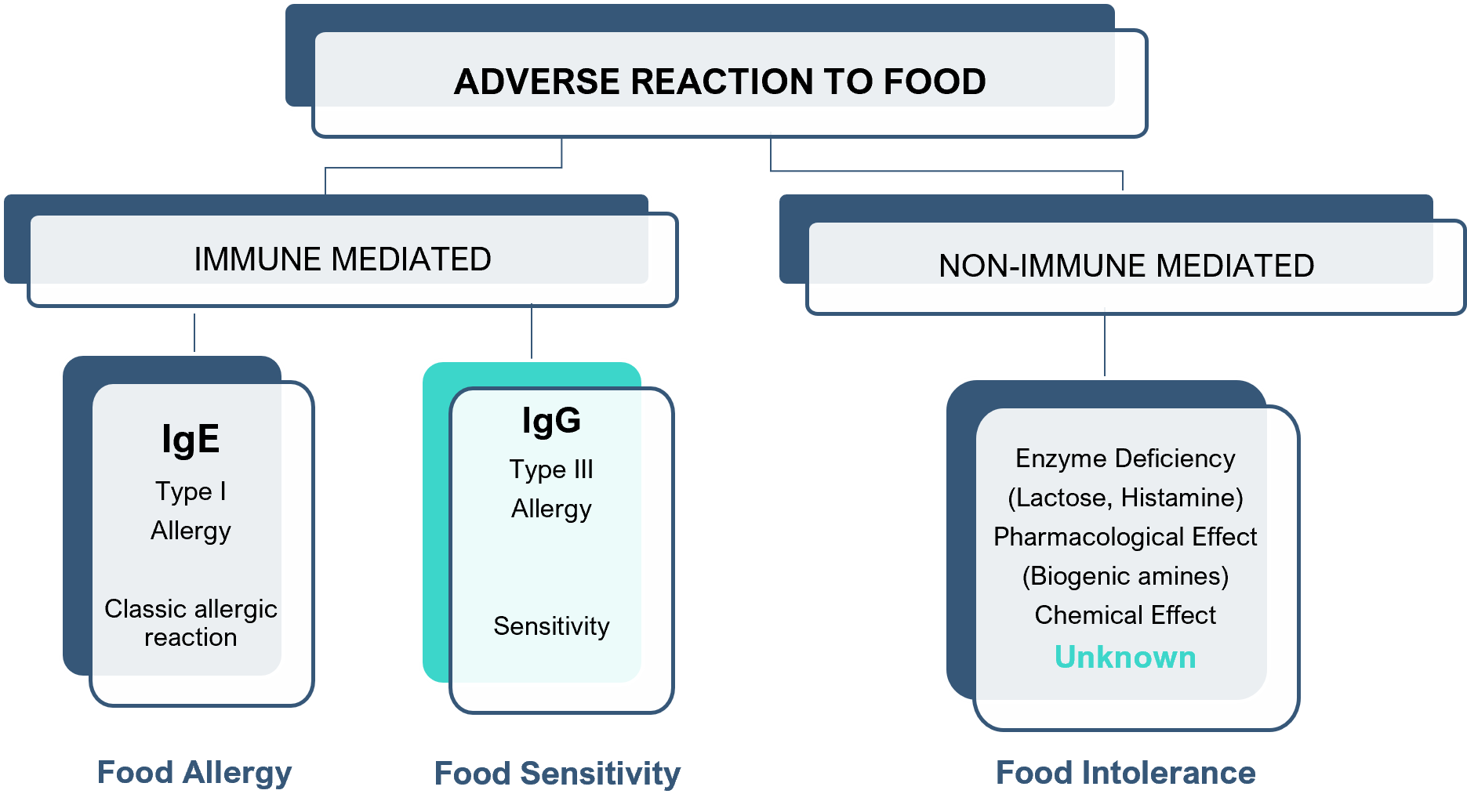
An immune reaction to food is an adverse response to a food component (allergen), which can provoke a variety of immune responses. There are two common antibodies associated with adverse immune reactions to food, IgE and IgG.
- IgE-mediated food reactions, type I hypersensitivity (classical allergy), are of immediate onset after exposure to food allergen. The adverse symptoms displayed are classically associated with an allergic reaction such as anaphylaxis.
- IgG-mediated food reactions, type III hypersensitivity, or food sensitivities, can occur several hours or days after exposure and can be caused by multiple allergens. Such reactions are associated with an inflammatory response which has been shown to be related to conditions such as Irritable Bowel Syndrome (IBS) and its associated symptoms (including bloating and diarrhoea) and migraines.
Food sensitivity is used for reactions to food which do not involve the immune system e.g. lactose intolerance, which is caused by an enzyme deficiency.
Intestinal permeability
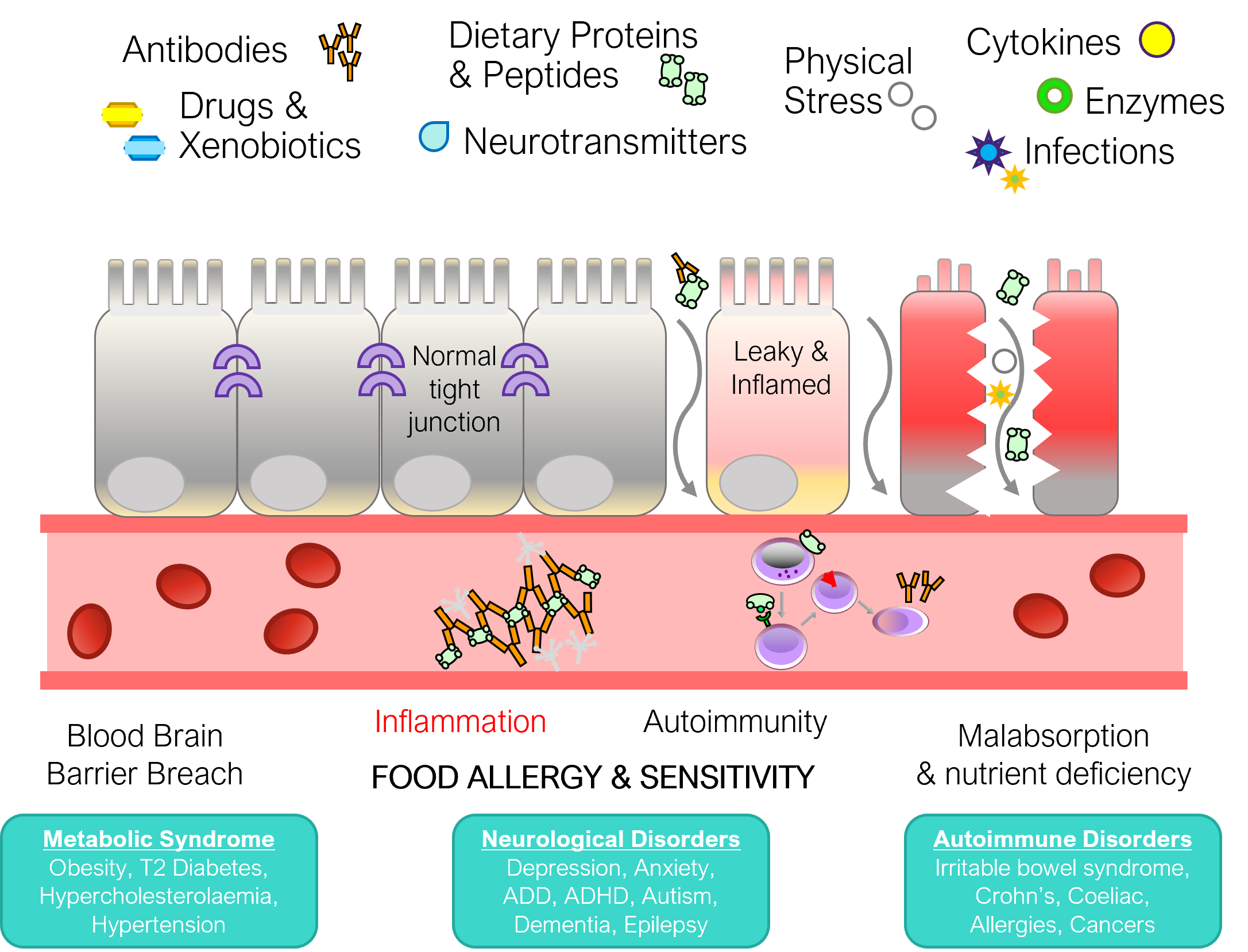
Evidence suggests that the development of IgG-mediated food sensitivity is directly related to increased permeability of the intestinal barrier. In a healthy normal intestinal tract where homeostasis is preserved, this barrier is tight and highly selective, so that only desired nutrients enter the bloodstream from the intestinal lumen, while access to potentially damaging substances and pathogens is impeded. Loosening of the barrier’s tight junctions makes it possible for larger particles – not only nutrients but also toxins, food allergens and microorganisms – to penetrate. The increased permeability of the intestinal barrier is often referred to as ‘leaky gut syndrome’.
There is increasing evidence that damage to the tight junctions and the subsequent influx of toxins and allergens leads to abnormal immune reactions and the potential development of autoimmune diseases.
A number of studies have shown that damage to the tight junctions is the precipitating cause for the development of food specific IgG antibodies. Furthermore, there is evidence that permeability is selective to food allergens. In a published review of all publications relating to increased permeability, IgG antibodies and IBS by Pasquale et al, in 2018. The authors concluded that the production of such antibodies is a specific reaction, rather than a non-specific reaction, as is widely believed.
Factors leading to increased gut permeability
- Antibiotics
- Medication / Drugs
- Candida overgrowth
- Parasites
- Intestinal infection
- Vitamin D deficiency
- Glutamine insufficiency
- Alcohol
- Poor diet
- Stress
- Low stomach acid
- Low pancreatic enzymes
Support with specific dietary and supplement protocols.
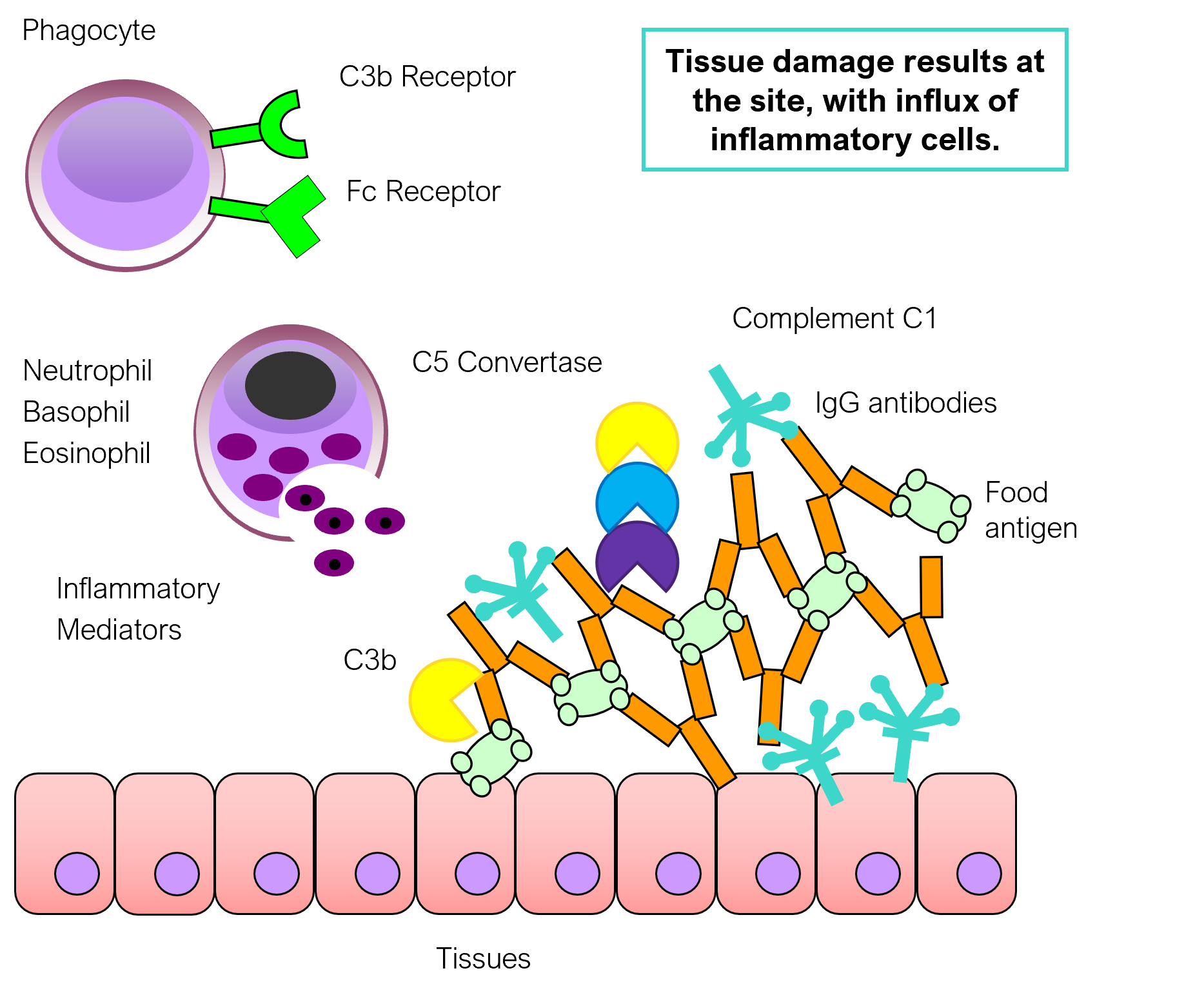
Inflammation
When elements that originate from the intestinal lumen enter the bloodstream an immune response is triggered. While this response is necessary to eliminate potentially harmful substances and microorganisms, such as pathogenic bacteria and viruses, it is potentially undesirable with respect to harmless neutral food particles. Ingestion of food may therefore lead to chronic activation of the immune system in which IgG antibodies are involved, leading to the development of immune complexes which in turn cause chronic inflammation and mechanical damage to the surrounding tissues.
Clinical manifestations
Controversy surrounds food IgG testing and this relates to the role food IgG antibodies play in the pathogenesis and diagnosis of food sensitivity and a number of chronic illnesses. However, elevated levels of IgG antibodies to food antigens have been observed consistently in diseases associated with increased intestinal barrier dysfunction. In addition, clinical studies have shown in some cases that there is a role for food IgG testing in certain conditions, such as IBS and migraines.
The clinical manifestations of chronic IgG-dependent reactions depend on the target tissue or organ to which the immune complexes, composed of IgG and the food antigens, are transported within the bloodstream.
Effects of elimination diet
Numerous studies specifically investigating the potential role of IgG food sensitivity in the pathogenesis of Irritable Bowel Syndrome (IBS) have been conducted. Atkinson et al. (2004) for example, showed that an elimination diet can be effective in relieving the symptoms of IBS. After 12 weeks of the diet, a 10% improvement in overall well-being and resolution of some symptoms was observed. Notably, in patients who decreased the restrictiveness of the diet, a 24% worsening of the symptoms was observed compared to patients strictly adhering to it.
Drisko et al. (2006) conducted a study in patients meeting the Rome II criteria for IBS, in which they followed a diet based upon the result of tests for IgG reactions to food for 6 months. This study showed abnormal levels of IgG antibodies to certain foods in all patients. Implementing a diet based upon the results led to a statistically significant improvement in symptoms.
The efficacy of a diet based on measuring IgG antibodies to food has been demonstrated in a number of conditions, both in independent studies and clinical practice. Excellent results have been obtained in patients with migraine and IBS. A diet based on food-specific IgG test results, has shown to be a safe and effective treatment for patients with these chronic conditions.
Conditions in which the presence of elevated food-specific IgG antibodies have been demonstrated:
| Symptoms associated with IBS | Symptoms associated with migraine |
| Bloating | Irritable bowel syndrome |
| Constipation | Lethargy |
| Diarrhoea | Migraine |
| Flatulence | Nausea |
| Headaches | Stomach cramps / abdominal pain |